LET US EVALUATE YOUR CASE
Dr. de Quintana will make an accurate diagnosis and explain the options to restore your quality of life.
+34 699 922 118 info@drdequintana.com location
SPINE SURGERY
Diseases that affect the spine are one of the
main causes of pain, impaired quality of life, and sick leave.
In expert hands and after a precise diagnosis, there are multiple alternatives
to eliminate pain and return to a normal life.
In routine clinical practice, if there are no alarming signs of disease state,
Dr. de Quintana proceeds with an approach which applies therapies from less to more.
Many patients can have their pain eliminated
with conservative or minimally invasive techniques.
PATHOLOGIES
HERNIATED DISC
FREQUENTLY LUMBAR OR CERVICAL
A herniated disc occurs when disc material (nucleus pulposus) comes out of its usual position. If this material is in contact with the nerve, it causes pain, which often radiates to the arm in cervical hernias and to the leg (sciatica) in lumbar hernias.
It should be taken into account that in more than 90% of the cases the condition resolves with conservative treatment, and with time, the herniated disc tends to be reabsorbed.
If there are alarming signs such as neurological deficit (for example, foot drop), or the pain does not improve and affects quality of life, ultraselective surgical techniques are recommended to free the nerve root and extract the hernia, which will lead to the disappearance of the pain.
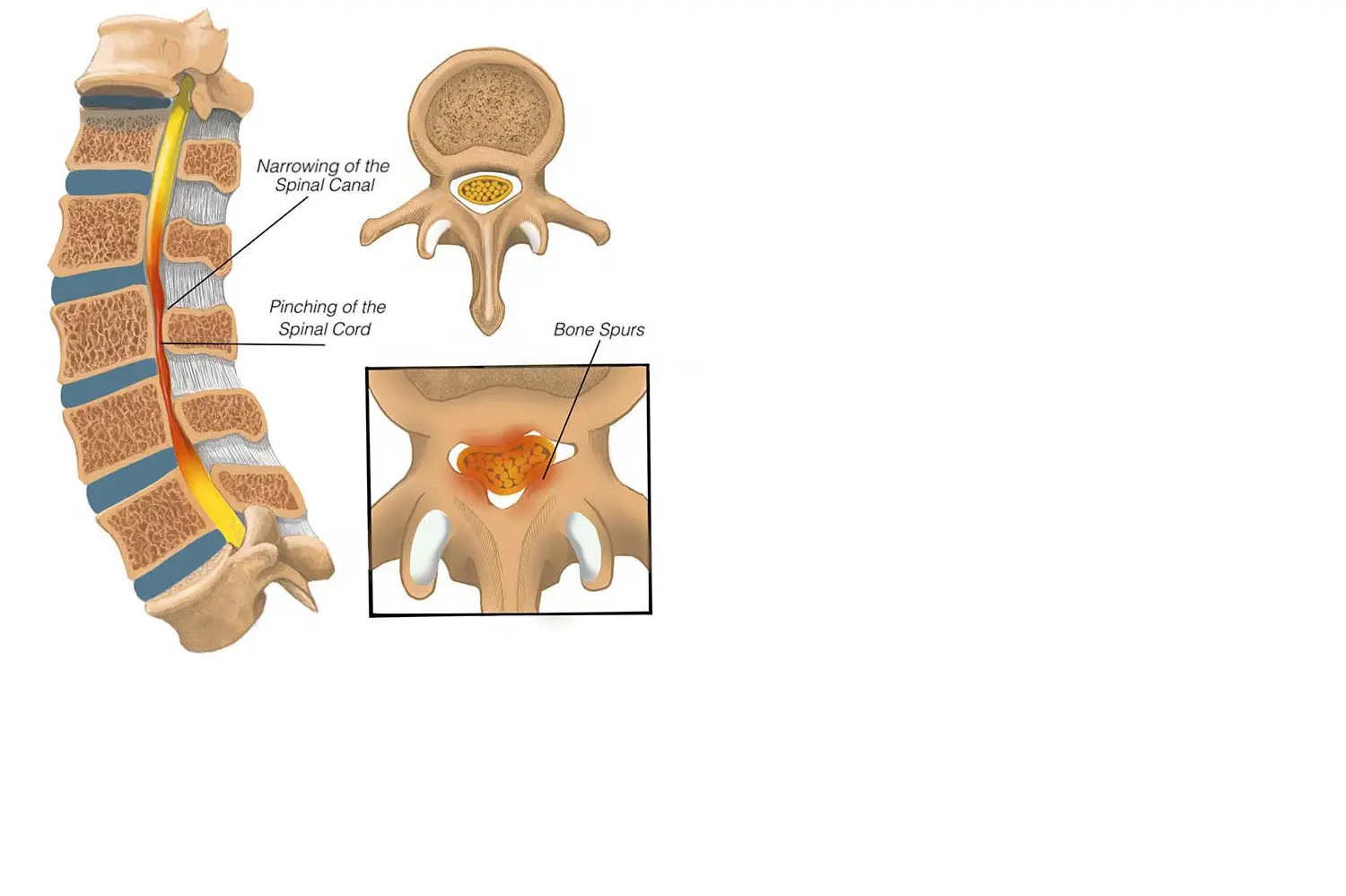
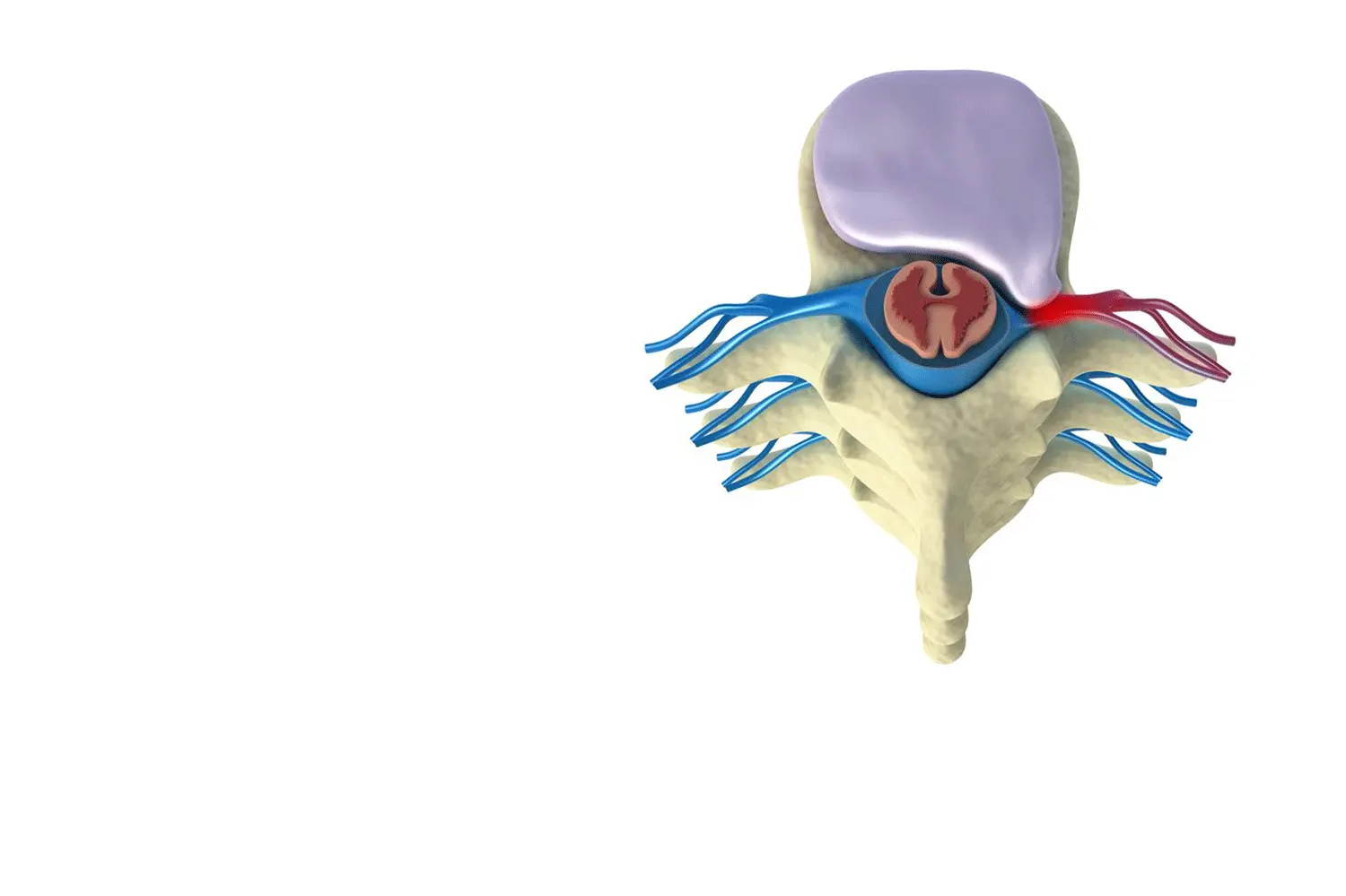
SPINAL STENOSIS
FREQUENTLY LUMBAR OR CERVICAL
This degenerative disease occurs when the central canal through which the spinal cord and nerves pass through narrows and consequently compresses the nerve structures.
At the lumbar level this classically causes what we call neurogenic claudication: the patient, when walking, has to stop due to pain in their legs and must sit down for a time before continuing. At the cervical level, spinal stenosis causes spinal cord compression leading to various symptoms, but the most frequent being pain and the sensation of lack of strength.
This pathology requires experience in diagnosis to offer the best treatment. At the surgical level, the objective is to decompress the nerves, which leads to an almost immediate improvement in the quality of life.

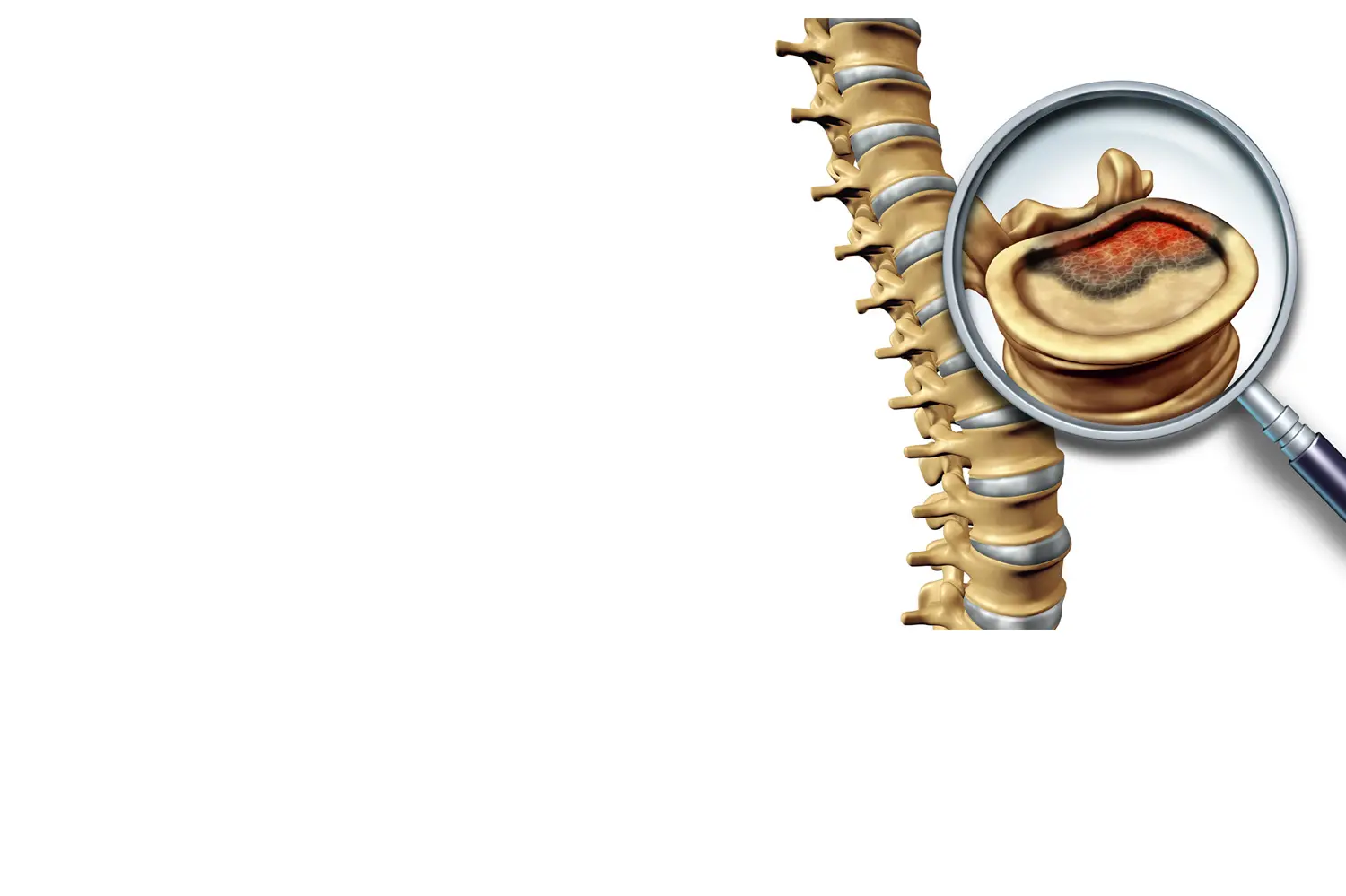
DISCOPATHY
DISC DISEASE
Over time the discs that act as cushions between the vertebrae can degenerate. This can cause back pain and sometimes even pain radiating to the arm (cervical) or leg (sciatica, lumbar). Discopathies are one of the most frequent pathologies in the general population and occur more frequently in patients with jobs that are or were demanding on the spine.
Our philosophy is that there is nothing better than your own disc, so our treatments are aimed at eliminating pain, while preserving the patient's disc. If all the more conservative techniques fail, as a last option, we have the surgical option that must be individualized for each patient:
- 1. Disc prosthesis (preserves the movement of the spine).
- 2. Fusion (when there is hypermobility of the segment).
FACET PAIN
JOINTS OF THE SPINE
The facets are the joints of the spine and together with the disc they support the spine. Jobs that are demanding on the spine - jobs that require prolonged sitting, standing still, or lifting weights - overload these joints and cause back pain. Classically it is a pain that worsens when sitting for a long time, standing still, or when getting up after sleeping. It is a type of pain that affects the quality of life and patients explain that they cannot do all the day-to-day activities that they would like to do.
The treatment of this pathology requires a precise diagnosis, and when the selected treatment is applied, (Example: Rhizolysis) it is very effective and patients can return to their normal life.
SPINAL TUMORS
THREE LARGE GROUPS
- 1 - EXTRADURAL-TUMORS: arise outside the nerve tissue but due to their growth they can compress the nerves. The most frequent type is Metastasis.
- 2 - INTRADURAL-EXTRAMEDULLARY TUMORS: arise within the meninges and usually form from the nerves themselves (Neurinomas) or from the meninges (Meningiomas).
-
3 - INTRADURAL-INTRAMEDULLARY TUMORS: arise from the spinal cord and the two most frequent types are Astrocytomas and Ependymomas.
These are tumors that can be extremely complex, requiring extensive experience in Neuro-Oncology and the latest technological advances to achieve complete resection with maximum safety.
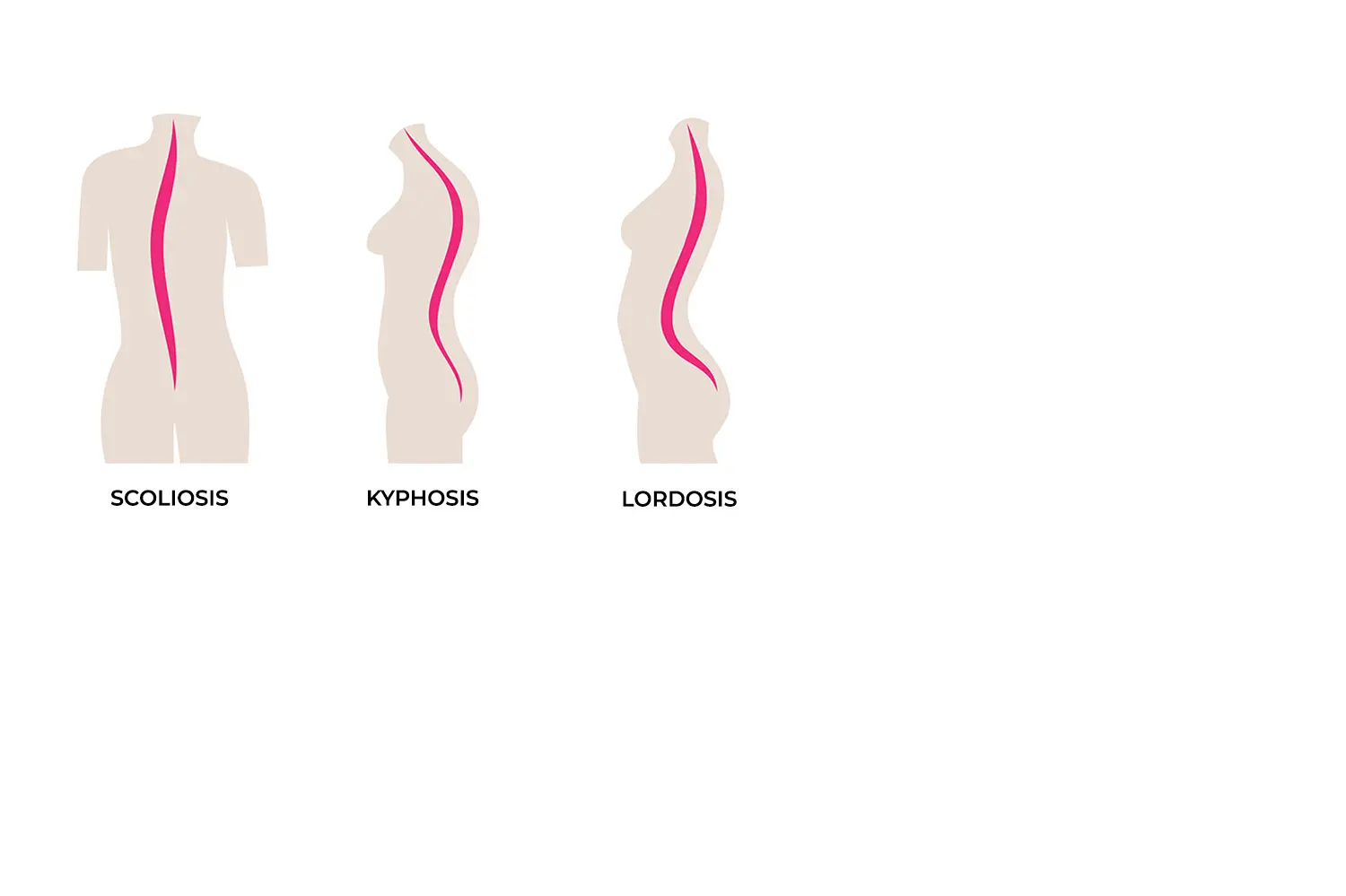
ALTERATION OF THE CURVATURE OF THE SPINE
SCOLIOSIS
Sometimes, this curvature is more accentuated when we are growing and in the stage of becoming taller. In this stage, the spine does not take on the optimal curvature and can deviate, causing the overload of different structures and pain.
In this pathology, muscle strengthening and postural therapy work is essential for significant improvement in pain. If, despite this, the pain persists or quality of life is affected, it is necessary to be very selective in the techniques used to improve the pain and not further alter the curvature of the spine.
In very few selected cases, surgery must be performed to reestablish the curvature of the spine.
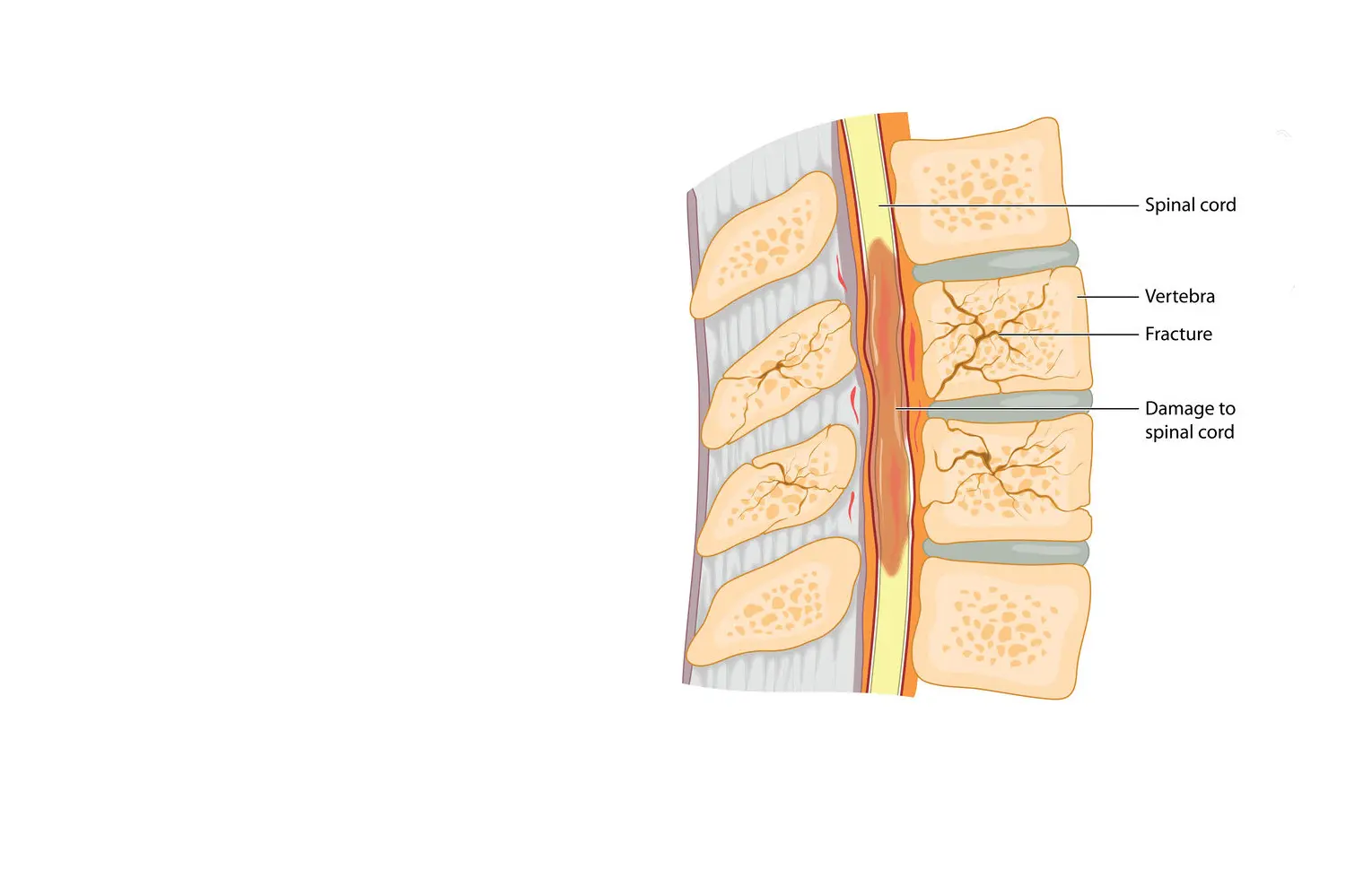
SPINAL TRAUMA
FRACTURE OF ONE OR MORE VERTEBRAE
Accidents (traffic, sports, etc.) or falls can fracture one or more vertebrae. In these cases, correct diagnosis is essential for assessing the stability of the spine and the integrity of the spinal cord and / or nerves. Once a precise evaluation has been carried out, an individualized treatment plan will be developed.
The treatments range from resting + brace + posterior rehabilitation, cementation of the vertebra, or different fusion techniques when there is instability.
The treatment plan has 3 objectives: preserve or recover the nerve function, stabilize the affected segment to avoid deformities, and eliminate the pain.
INNOVATION
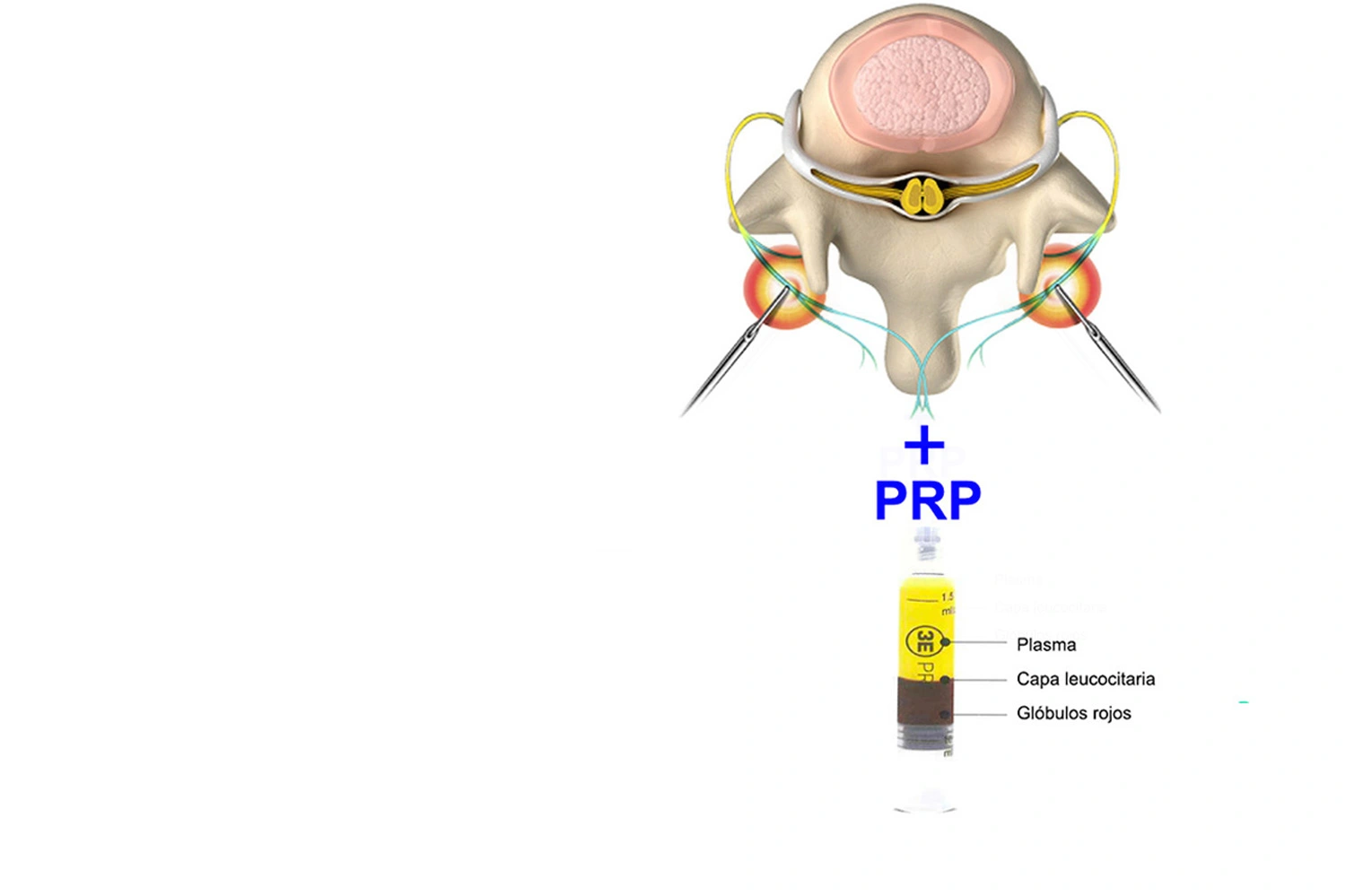
RHIZOLYSIS + PRP
ELIMINATE FACET PAIN AND REGENERATES JOINTS
Rhizolysis is a very effective technique that eliminates pain coming from the joints of the spine (facet's pain).
It is an outpatient procedure (no admission required), with great effectiveness and safety.
Currently, we are not only seeking to eliminate that pain. There are some techniques that also try
to regenerate those joints.
PRP (Platelet Rich Plasma) is obtained by centrifuging the patient's own blood
and can be injected into the facets during the same procedure. The function of these growth factors is to
restore the spinal joint and reduce inflammation so that the beneficial effects of rhizolysis last longer.
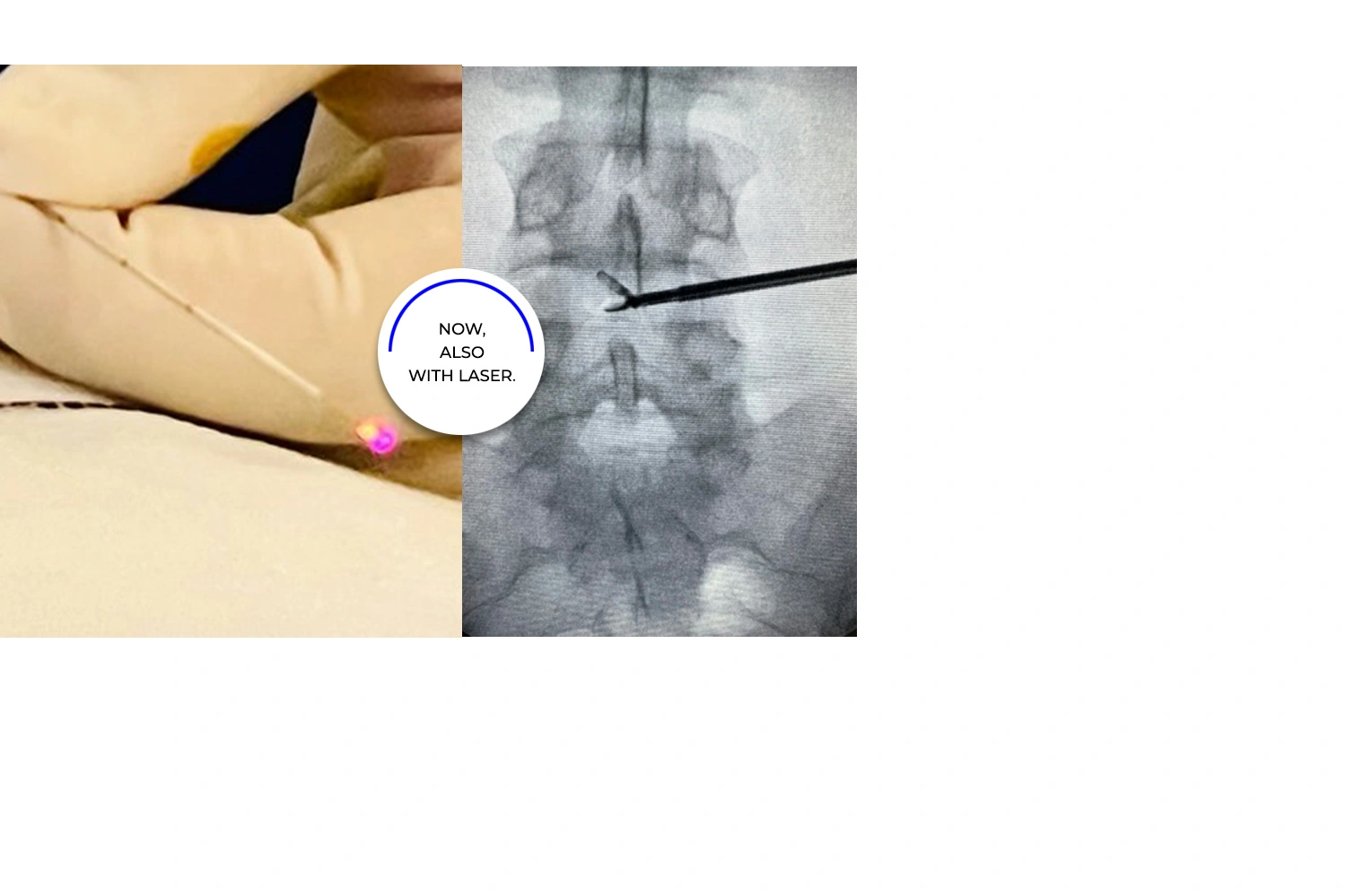
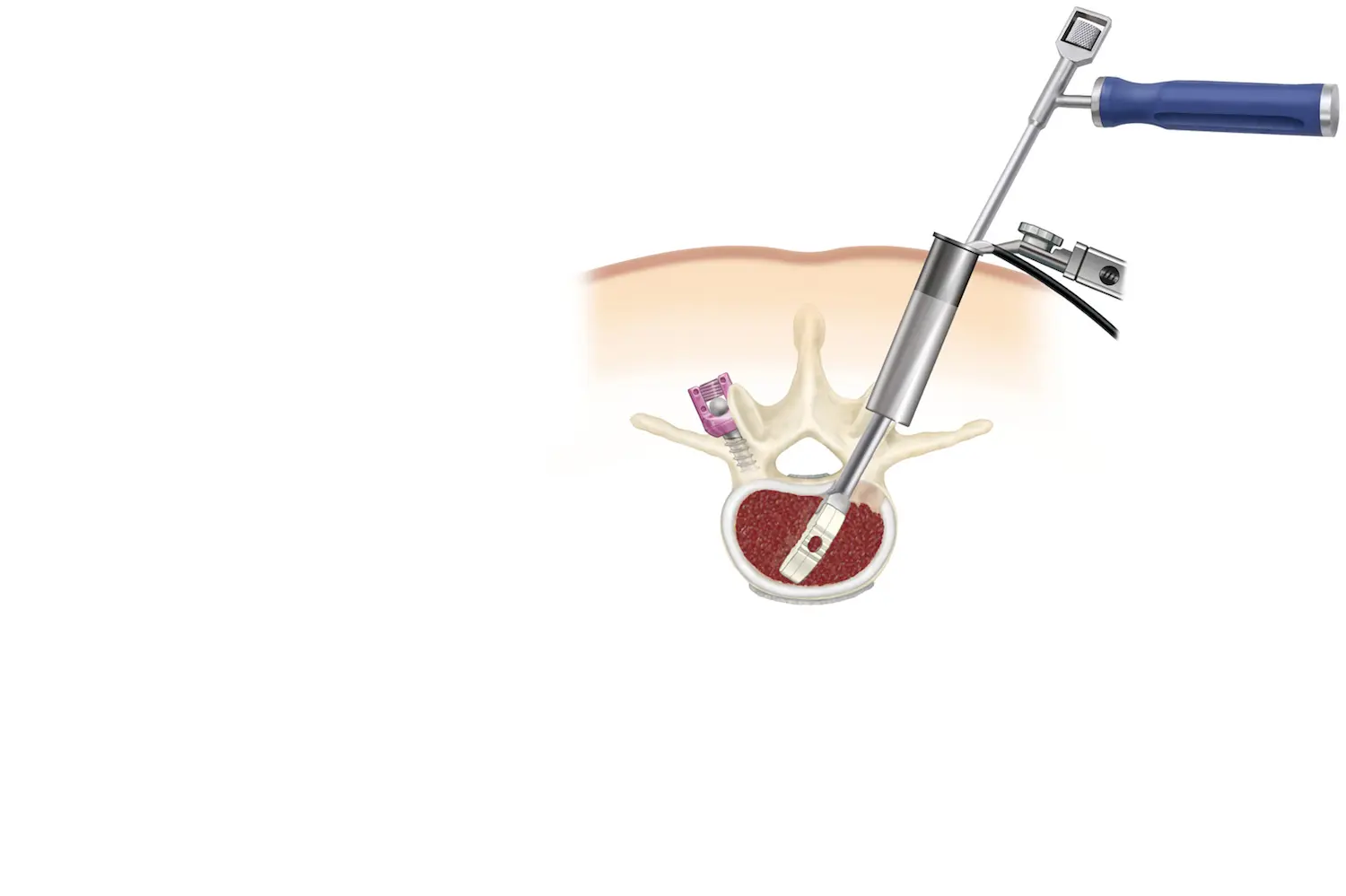
DYSCOLYSIS
IMPROVING THE PAIN THAT COMES FROM THE DISC
Discolysis is a procedure aimed at improving the pain that comes from the disc.
In addition, through the cannula with which we work we can even extract herniated discs and expand the channel as we can see in the photograph.
It is a technique that requires experience in pain treatment and minimally invasive techniques to achieve the best results.
MINIMALLY INVASIVE SURGERY
ALTERNATIVE TO CLASSIC SPINE SURGERY
An alternative to classic spine surgery is to employ minimally invasive techniques. This set of techniques is aimed at performing the same procedure that would be done in the classic way but through small incisions and using dilators. This allows us to preserve the muscles of the spine, minimize blood loss in surgery, reduce postoperative pain, and accelerate recovery from surgery.
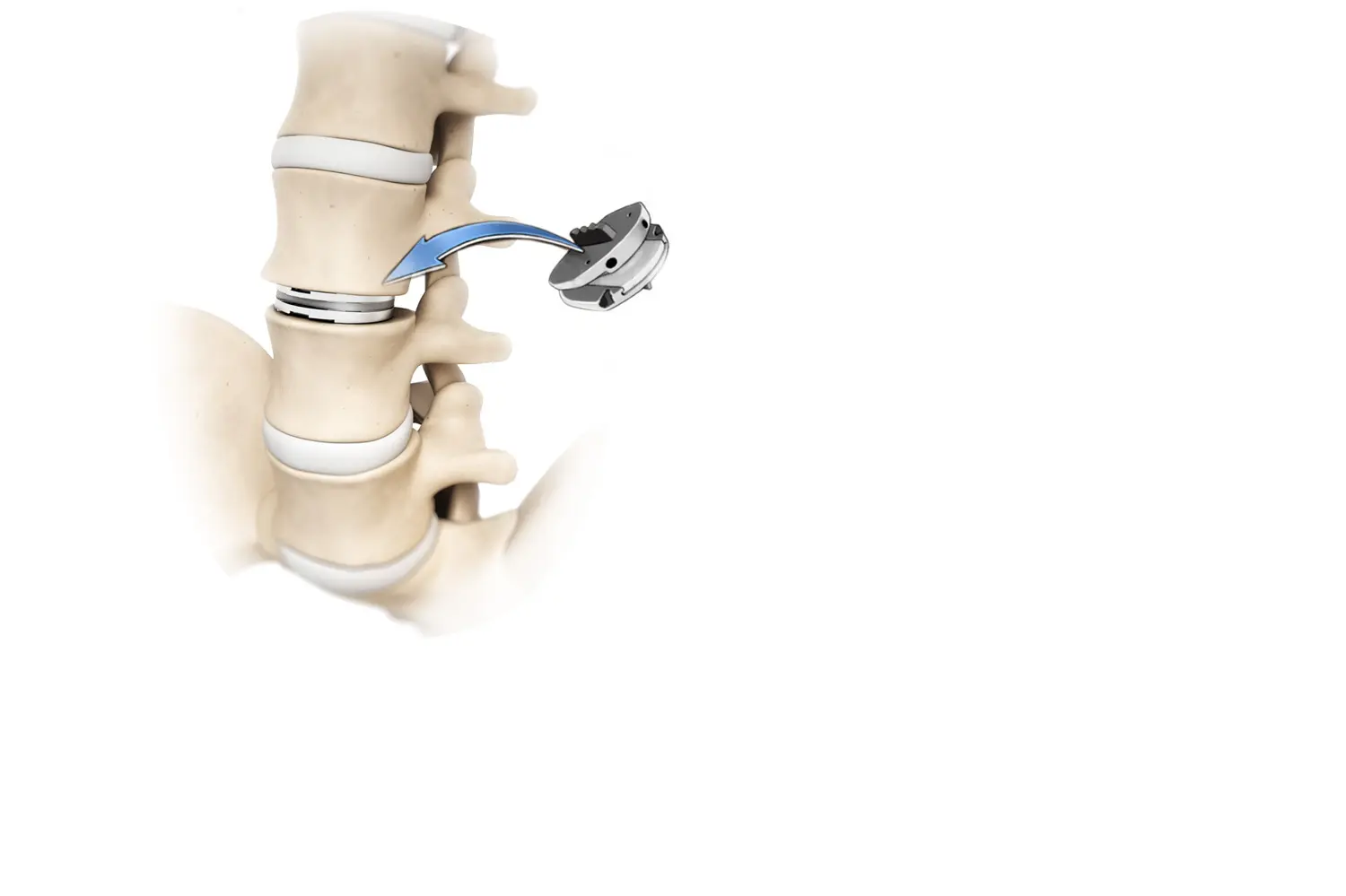
DISC PROTHESIS
VERTEBRAL DISC REPLACEMENT
Sometimes the spinal disc is so affected that it requires replacement.
Disc prostheses are a great therapeutic tool since they allow us to replace the disc while preserving the movement of the spine.
At the cervical level this is a widely used technique. However, at the lumbar level the approach is more complex, operating here involves a learning curve, so choosing a doctor with experience will ensure the best possible results.
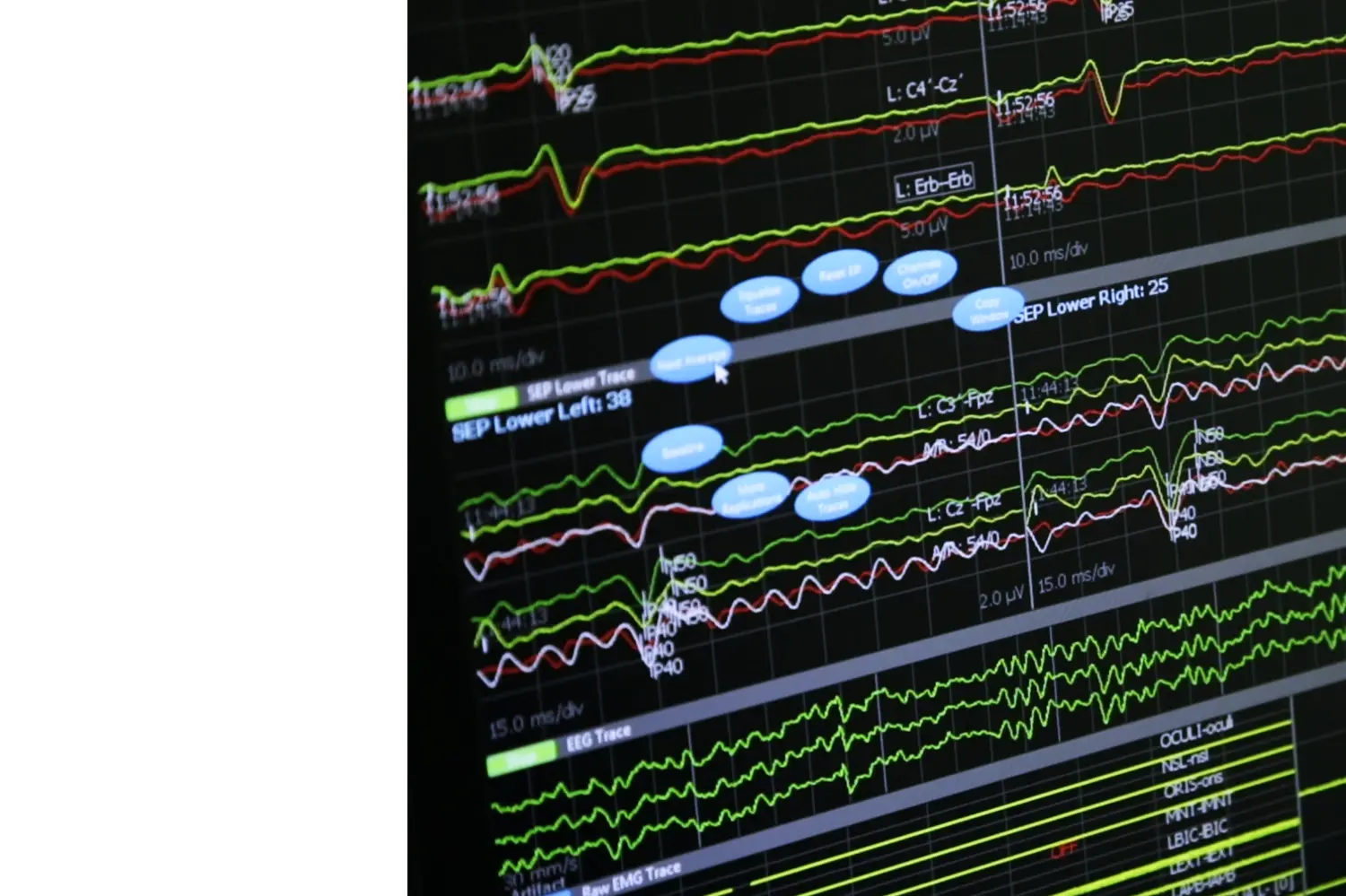
INTRAOPERATIVE NEUROPHYSIOLOGY
EVALUATE THE SPINAL CORD AND NERVES
Spinal operations must be safe, and we achieve this through intraoperative neurophysiology.
During surgery, the neurophysiologist performs motor and sensory stimulations that allow us to evaluate the spinal cord and nerves intraoperatively to avoid damaging them. This is a critical technique to employ when operating on spinal cord conditions and recommended for the control of nerve roots.
Extensive experience and coordinated teamwork between the neurosurgeon and the neurophysiologist is required for the correct interpretation of the data.
OTHER TECHNIQUES
- Neuronavigation (column GPS).
- Endoscopic surgery.
- Ozone therapy.
- Navigated ultrasound for spinal tumors.
FAQ´S
- Wound: requires daily cleaning + dressing. The stitches are usually removed after 7-10 days depending on the patient’s progress.
- Medication: follow the instructions of your neurosurgeon for the treatment of pain and inflammation.
- Follow-up visits: your doctor will usually schedule a visit 7-10 days after the operation to remove the stitches. The next follow-up is one month after surgery, often with an X-ray. Subsequently, the intervals of the follow-up visits may vary according to the patient’s progress.
- Rhizolysis pain technique: does not require hospital admission, it is an outpatient patient procedure.
- Simple disc herniation: 2-3 days.
- Instrumented spinal surgery (example: spinal fusion): 5-6 days.
Broadly speaking, we need at least one month for the muscles to heal and then it is advisable to carry out rehabilitation for a minimum of two weeks and ideally one month. So, the average sick leave is 1.5 - 2 months, but this can be highly variable since sometimes more rehabilitation time is required to prepare the patient for work activity.
For a surgery for a simple herniated disc, this is not necessary although sometimes I recommend it just for greater safety to the patient and to better control the pain.
The brace is usually worn for a month and then if the x-rays look good, the brace can be gradually worn less and less.
It is not advisable to wear the brace for longer than this time since its chronic use atrophies the muscles.
When a cage is implanted (fusion) it is necessary to wear a rigid neck brace during the day and a soft one at night. A month after the surgery, we repeat an X-ray and if the healing progress looks correct, the neck brace can slowly be worn less and less after that point.
As in the previous question, it is not advisable to wear the neck brace for longer than this time as it can atrophy the muscles.
LET US EVALUATE YOUR CASE
Dr. de Quintana will make an accurate diagnosis and explain the options to restore your quality of life.
+34 699 922 118 info@drdequintana.com location